About the Da Vinci Project
Interoperability challenges have limited many stakeholders in the healthcare community from achieving better care at lower cost. The dual challenges of data standardization and easy information access are compromising the ability of both payers and providers to create efficient care delivery solutions and effective care management models. The goal of the Da Vinci project is to help payers and providers to positively impact clinical, quality, cost and care management outcomes.
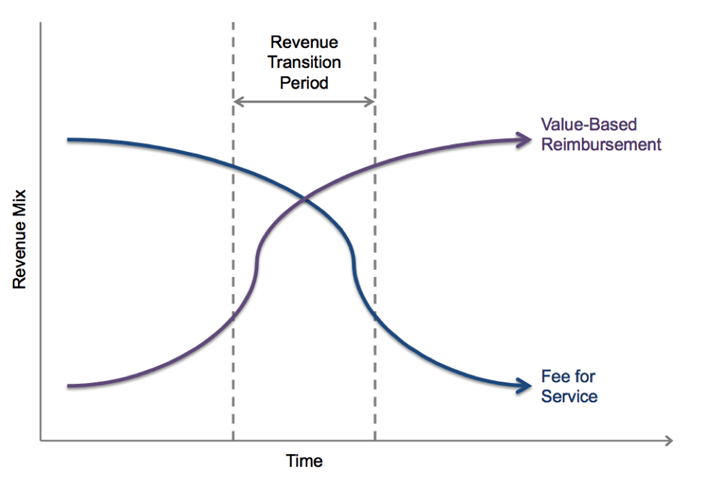
Value Based Care Programs Drive Focus to Patient Outcomes by enabling providers to see the right data at the right time for patient-centered care… in terms of specific patient coverage, their benefits and effective care coordination. Historically, payment and coverage data were completely separate from care.
Da Vinci stakeholders are industry leaders and health IT technical experts who are working together to accelerate the adoption of HL7 Fast Healthcare Interoperability Resources (HL7® FHIR®) as the standard to support and integrate value-based care (VBC) data exchange across communities.
Want to publish your own articles on DistilINFO Publications?
Send us an email, we will get in touch with you.
Empower End Users to Shift to Value: As a private industry project under HL7 International, Da Vinci will unleash critical data between payers and providers required for VBC workflows leveraging HL7 FHIR.
Da Vinci responds to a need to establish a rapid multi-stakeholder process for addressing value-based care delivery use cases that can be implemented on a national basis. The objective is to minimize the development and deployment of unique solutions between trading partners (e.g. a payer and provider). To promote interoperability across value-based care stakeholders and to guide the development and deployment of interoperable solutions on a national scale, the industry needs common:
- Standards (FHIR)
- Implementation guides
- Reference implementations
Members have established a governance model that will ensure equal representation from stakeholders and offer transparency. Funding members will have the ability to focus priorities for industry progress and meet the overarching goal to improve appropriate clinical and metrics data sharing between providers and payers. The founders represent a diverse body of stakeholders with experience across the specific VBC business challenges, emerging FHIR standards and practiced at agile development. Founding organizations are drawn from payers, providers and vendors committed to making value-based care a reality.
Timeline
- Da Vinci demonstrates progress at HIMSS2019
- January 2019 Da Vinci members add three new uses cases:
- Gaps in Care & Information
- Risk Based Contract Member Identification
- Alerts: Notification (ADT), Transitions in Care, ER Admit/Discharge
- November 2018 Da Vinci members added Prior Authorization Support use case
- Fall 2018 initial two use case Implementation Guides were balloted at HL7. Both Guides and Reference Implementation Materials are available on the Da Vinci Confluence Page.
- In Summer 2018 the membership added three additional use cases:
- In January 2018 stakeholders approved the formation of Da Vinci and work began on the initial use cases. Da Vinci members identified payer/provider trading partners to develop and validate the artifacts and tools for two targeted use cases in 2018.
Source: HL7







